Over the last several years, rapid digital transformation has taken center stage in the healthcare payer space. But as new technologies are adopted and implemented, that focus is shifting to growth, member experience, and technology optimization. According to the 2023 Gartner CIO and Technology Executive Survey, healthcare payers are shifting technology investment priorities to establish a shared enterprise digital vision. Still, challenges remain in achieving consensus and developing a clear action plan.
In this article, we dive deeper into the survey results and what they mean for health plans and healthcare technology spending in the coming year.
Changing Healthcare Payer Priorities
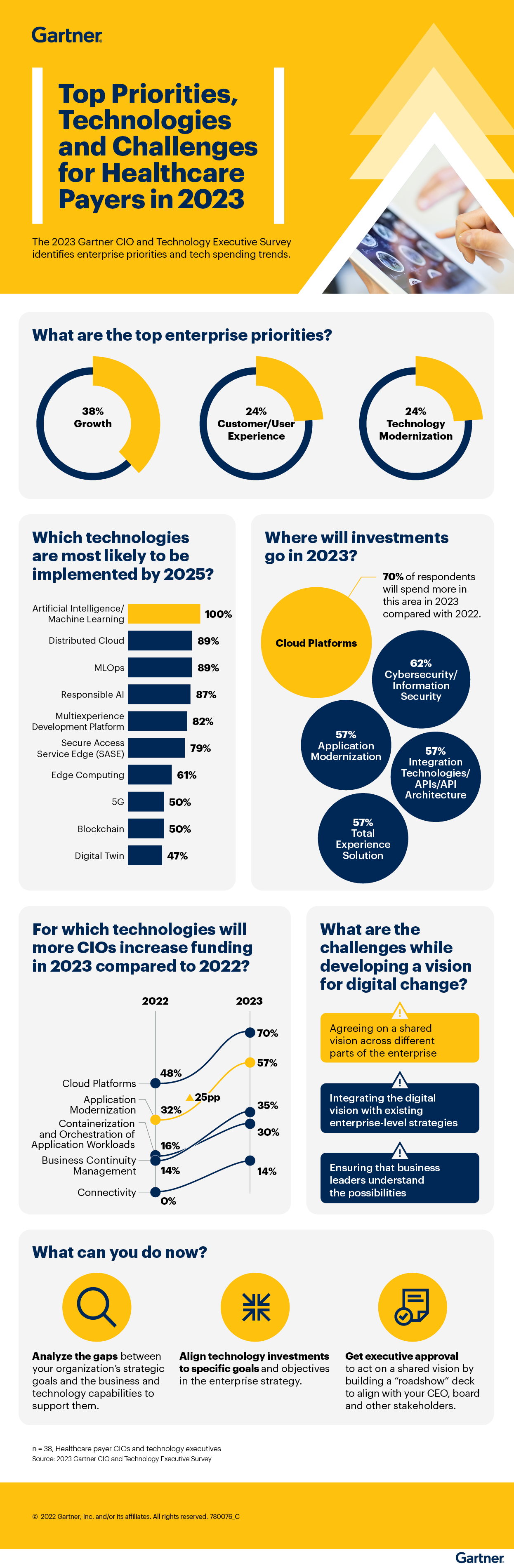
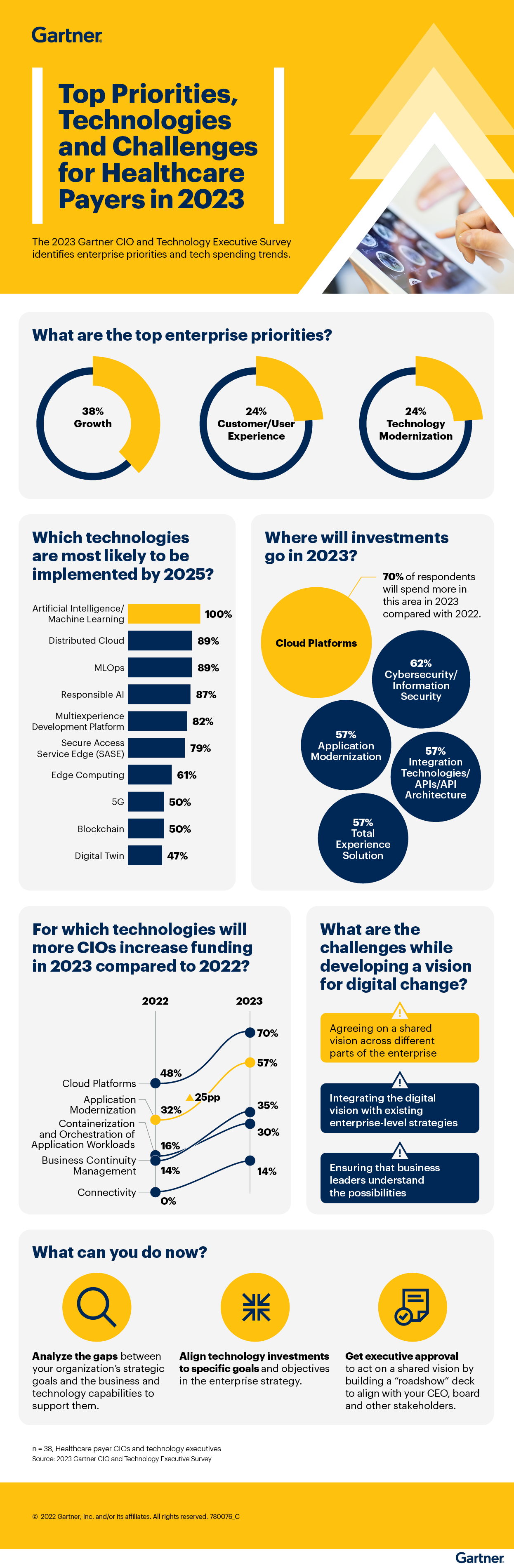
Growth, member experience, and technology modernization are the top three healthcare payer enterprise priorities going into 2023, according to the Gartner survey, with 38%, 24%, and 24% of top responses, respectively. Health plans understand that members want more from their healthcare experience and are looking at priorities through the lens of health equity and the digital patient experience. Member empowerment is a crucial payer imperative, and health plan technology investments are increasingly being earmarked for tools that directly and indirectly enhance the member experience.
While also a top priority, technology modernization remains a challenge for payers struggling to reconcile new technologies with existing enterprise strategies and dependency on legacy systems. As such, investments are increasingly going toward integration technologies that help bridge the gap between current and new solutions.
Artificial Intelligence, Cloud Technologies Top Payer Implementation Plans
Largely spurred on by the shift toward consumerization and value-based care, artificial intelligence (AI) has transitioned from early to mainstream adoption when it comes to healthcare payers’ implementation plans. A complete 100% of Gartner survey respondents indicated they are likely to implement AI/machine learning by 2025, with related technologies such as responsible AI and MLOps also planned for adoption.
According to Holly Toomey, Vice President of Product at Vital Data Technology, “It has become imperative for our payer clients to leverage the benefits of the digitally connected healthcare ecosystem to provide efficient and integrated care.” She continued, “Our large health plan client’s adoption of AI and predictive analytics has enabled them to identify and intervene with certain high-risk members much sooner and more effectively than ever before. This outcome shift is truly eye-opening for everyone in the ecosystem and points to the transformative effect of these technologies.”
Payer spending in 2023 is expected to increase dramatically for cloud-based platforms, with 70% of payer executives saying they will spend more in this area than in 2022. Application modernization also ranks high, with 57% of payer executives responding they will spend more in 2023. This modernization spending focus is due, in part, to ongoing legacy dependence - acting as a workaround of sorts to true innovation and digital progress.
“We recognize that our health plan clients aren’t necessarily at the point where they can simply rip and replace a legacy system,” said Toomey, “that’s why our cloud-native, purpose-built solutions are API-driven, modular, and flexible. In this technology modernization and optimization environment, no single solution will necessarily be the be-all, end-all for a health plan. Applications must work together to provide an integrated solution.”
Shared Digital Vision Remains a Challenge for Payers
Despite the desire to implement time and cost-saving technologies, challenges remain across the enterprise to develop a unified vision for digital change. According to the Gartner survey, the most significant challenges include the following:
- Agreeing on a shared vision across different parts of the enterprise
- Integrating the digital vision with existing enterprise-level strategies
- Reconciling modern technologies with existing enterprise strategies
- Ensuring that business leaders understand all the possibilities
To address these challenges, Gartner recommends health plan stakeholders work to align technology investments to specific goals in the enterprise strategy. They need to analyze the gaps between these goals and the organization’s ability to provide the technology required to support them. At Vital Data Technology, we believe a cloud-native, modular platform that provides seamless integration across medical management departments is a step in the right direction.
Vital Data Technology is committed to helping health plans of all sizes transform data into actionable insights using AI and advanced analytics integrated with embedded HEDIS® and risk adjustment logic. Our Affinitē platform is purpose-built and flexible, deployed as a cloud-based, end-to-end solution. It is also available through distinct modules to help payers with their medical management needs across Care Management, Utilization Management, Quality Improvement, Risk Adjustment, Care Gaps, and Data Science.
For more survey results, please refer to the Gartner infographic below.