The coming evolution of Centers for Medicare & Medicaid Services (CMS) Star Ratings marks a fundamental change that demands immediate attention from Medicare Advantage (MA) plans. With an increased focus on clinical performance, beneficiary experience, and equitable care outcomes, the upcoming changes present both obstacles and opportunities for health plans. To succeed in this new environment and boost Star Ratings, health plans must invest in advanced analytics, holistic strategies, and collaborative partnerships to optimize their operations and improve care delivery. In this article, we explore some of the ways that health plans can navigate and prepare for these coming changes.
A Refined Focus on Clinical and Experience Measures
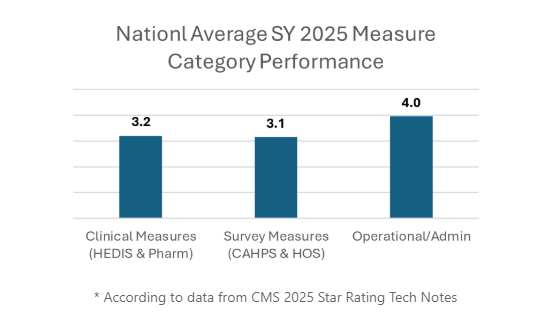
CMS is moving toward a streamlined measure set, shifting weight to clinical and experience-based outcomes. By 2026, clinical performance measures such as HEDIS and Pharmacy will carry 45% weight, while survey-based measures like CAHPS and HOS will account for 40%. Operational measures with historically high performance, like those related to SNPs, are being retired.
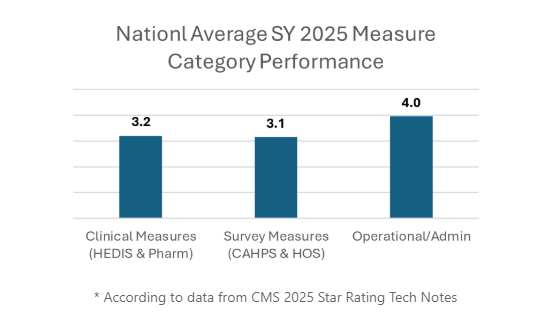
This adjustment aims to reduce administrative burdens and align quality measurement efforts. However, the shift also intensifies pressure on health plans. Clinical and survey measures have lower national averages—at 3.2 and 3.1 stars respectively (excluding SNP data) - which means excelling in these critical areas will require targeted focus. The success many health plans relied on from high-performing operational measures is no longer guaranteed.
The Tukey Method's Impact on Star Ratings
The implementation of the Tukey Method is set to significantly influence Star Ratings by providing a more robust statistical approach to identifying outliers in performance data. This method will enhance the accuracy of ratings by ensuring that extreme values do not disproportionately affect overall scores. As a result, health plans will need to focus on consistent performance improvements across all measures to maintain or enhance their ratings. By minimizing the impact of anomalies, the Tukey Method encourages a more stable and fair assessment of health plan quality, ultimately driving plans to prioritize sustained excellence in care delivery.
Transitioning to Electronic Clinical Data Systems (ECDS)
CMS is accelerating the transition to Electronic Clinical Data Systems (ECDS) reporting to improve interoperability and lessen reliance on manual processes, such as chart reviews. ECDS not only simplifies data collection but also provides real-time insights that can improve member outcomes. Still, the shift comes with a steep learning curve as plans must modernize their infrastructure and processes:
- Data preservation and integration: Plans need robust IT systems to manage historical and supplemental data for seamless access and usage.
- Proactive chart reviews: Off-season chart reviews can help close data gaps ahead of deadlines, allowing plans to stay ahead of issues.
- Provider collaboration: Engaging providers to align data capture workflows ensures both better compliance and more meaningful health outcomes.
This may require increased investment in tools and technology to aid in the ECDS process. However, health plans that adopt ECDS successfully can not only meet new requirements but also leverage actionable insights to enhance care delivery.
CAHPS and HOS Take Center Stage
Survey measures, particularly CAHPS and HOS, are becoming even more pivotal in determining Star Ratings. CAHPS evaluates member experience regarding access to care, interactions with providers, and health plan operations, while HOS focuses on long-term health outcomes and serves as a measure of whether physical and mental health has been maintained or improved.
The stakes are rising, with HOS measures increasing to a 3x weight by 2027, according to CMS. And the potential expansion of HOS denominators to include Medicare Advantage members aged 18 - 64 could create added challenges. The younger end of this cohort historically shows lower engagement and more complex mental health needs, potentially driving performance averages even lower.
In addition to ensuring member engagement is a top priority for plans, they must also adopt a year-round focus on improving member experience, address barriers to access, and collaborate effectively with providers. The days of treating CAHPS and HOS as isolated initiatives are gone; these metrics are now central to program success.
Addressing Health Equity and Behavioral Health Challenges
CMS is also prioritizing health equity and behavioral health initiatives, introducing measures like depression screening and follow-up as well as substance use treatment engagement. This reflects a broader intent to address longstanding disparities in care delivery. Yet, integrating such measures poses challenges, particularly in states with systemic barriers to behavioral health data sharing.
Health plans must work closely with behavioral health providers to develop reliable data-sharing systems and eliminate operational silos. Investing in holistic, state-specific solutions can mitigate regional disparities, ensuring equitable outcomes across diverse member populations. In addition, predictive models that help determine the timing and risk for developing certain mental health issues can help plans get out in front of potential issues.
The Competitive Edge of Advanced Analytics
Successfully navigating these changes requires more than just internal effort; it demands a high level of technological sophistication and the establishment of strategic partnerships. In today's rapidly evolving healthcare landscape, advanced analytics platforms and robust data integration capabilities have transitioned from being mere "nice to have" features to becoming absolutely essential for survival and success. These tools are critical in enabling health plans to not only keep pace with the dynamic regulatory environment but also to thrive within it.
For instance, vendor partners who specialize in the aggregation of disparate data sources, the delivery of predictive analytics, and the identification and addressing of quality gaps play a pivotal role in empowering health plans. These partners provide the necessary expertise and technological support that allow health plans to make well-informed, data-driven decisions.
By leveraging such advanced tools and forming the right partnerships, health plans can position themselves to not only meet but exceed the expectations set by the evolving healthcare regulations.
Preparing for the Future
The shift toward outcomes-focused Star Ratings underscores the urgency of transformation in Medicare Advantage programs. While CMS frequently changes rating criteria, leaders can utilize a data-driven approach that promotes agility across the organization and helps teams be prepared to manage upcoming changes without sacrificing quality.
Plans that invest in advanced analytics, prioritize health equity, and integrate the member experience into daily operations will find themselves well-positioned to lead. With the right strategy - and the right partnerships - these challenges can represent not hurdles, but opportunities to improve care and achieve long-lasting success.